Have Chronic Back Pain? It Might Be Sciatica
By Paul H Le, M.D.
About 35% of the population over 40 will have back pain, many of which is chronic pain.
There are all different types of back pain, but one of the more common ones is Sciatica. By learning more about signs and symptoms, it’ll be easier for you to get help early on so you can treat your pain easier.
Read on to learn more about a common back pain that radiates all the way down to your legs and what you can do if you think you’re suffering from it.
What is Sciatica?
Essentially, Sciatica is radiating pain, typically down the leg, secondary to irritation of the nerve root in the back.
That irritation is due to a slipped disc, a bulging disc, or spinal stenosis in the lumbar spine.
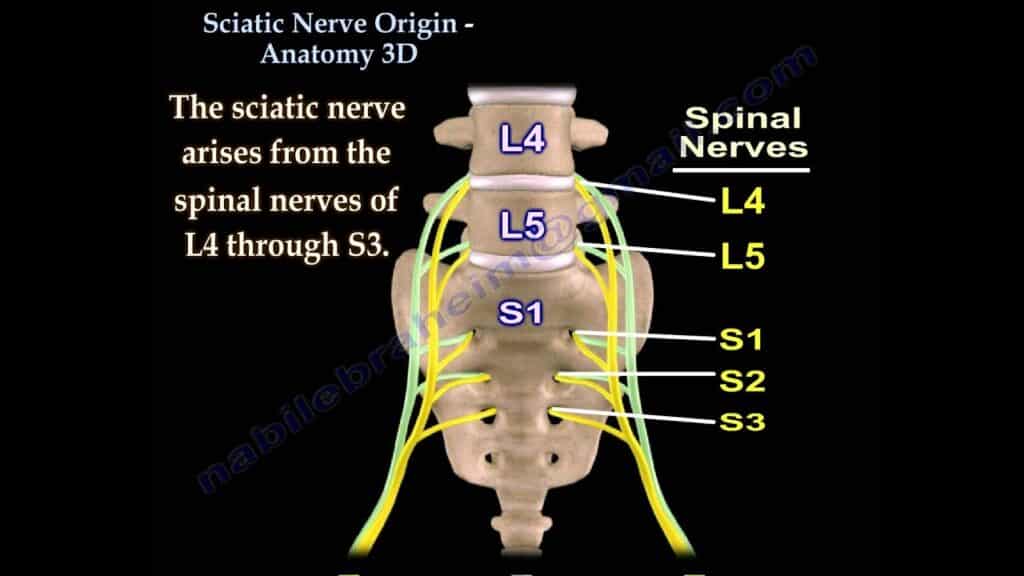
The lumbar spine comprises five vertebrae, each having a nerve that comes out below it. Each nerve leaves the spine, comes back together in the sciatic nerve, and travels down the leg.
Typically, depending on what level of disc bulging or spinal stenosis a patient is at, they might end up irritating or causing inflammation along one of the nerves.
The symptoms you’ll have in the leg are usually correlated to which nerve is irritated. Knowing where a patient is feeling their pain is helpful for us to figure out which nerve is experiencing inflammation or irritation.
For example, if a patient says they’re feeling chronic back pain, but specifically pain that’s radiating down the back of their legs down to their foot, it’s usually attributed to irritation in the L-5 nerve (the last nerve).
If another patient says they’re feeling pain in the front of the leg, it’s probably a higher-up nerve, like an L-3 or L-4.
It’s mimicking your body’s signaling pathway.
We have sensory fibers and nerves that dictate motor functions in the leg. When you irritate that nerve, you’re irritating the signaling pathway, which will mimic the irritation.
Related: Chronic Pain Can Occur At Age Age– How Yolanda Overcame Hers
How Do You Get Sciatica?
As we age, the discs in between the vertebrae get flatter and wider, making the hole where the nerve exits smaller and tighter. Depending on the activity you did to cause it, you might start rubbing or pinching that nerve, which causes it to get inflamed and creates symptoms down the leg.
You can also get Sciatica through an accident, an injury, or repetitive overuse. If you’re lifting heavy objects for your occupation, you might be experiencing pain sooner than someone who lives a more sedentary lifestyle.
As we get older, a lot of sciatic pain comes from “regular wear-and-tear”. But if somebody who’s relatively young had an accident and feels a pop, that’s when we know it’s due to the accident and not a more gradual process.
How Do You Treat Sciatica?
When we treat chronic back pain, but primarily Sciatica, we’re not necessarily eliminating the flattening of the vertebrae, but rather eliminating the symptoms and pain that comes with it.
We can sometimes improve people’s body mechanics and thus their pain through physical therapy, weight loss, or a lifestyle change. Here at APC, physical therapy is often the first option because it’s the most non-invasive.
Each patient requires different treatment based on their history with the pain, their symptoms with their current, and their pathology.
We’ll start with conservative treatments: using anti-inflammatories, heat, ice, rest, and physical therapy. The thing about most of our patients when they come in for Sciatica is that they’ve already exhausted these options at home or with their primary care physician or outside doctors.
If they’ve undergone treatment but don’t have a fundamental understanding of the injury, we’ll get imaging done first so we know the true nature of the problem.
From there, our treatment is customized per patient:
- If they’ve already gone for physical therapy, we might be able to offer them more customized physical therapy now that we know more about the injury after having the MRI.
- If they’ve “failed” conservative therapy because they didn’t do it, meaning taking an Ibuprofen or Aleve and leaving it at that, we might need to get them on a more regular schedule.
- If physical therapy didn’t help, we might prescribe oral steroids, the Cadillac of anti-inflammatories. That’ll give them a boost to get rid of inflammation, which is sometimes all they need.
- If they failed all of this, we’d try an epidural steroid injection.
Related: Myth Buster: Do Painkillers Reduce Your Pain Threshold?
The epidural steroid injection is a needle-based procedure where we take a needle under X-ray guidance, targeting the end of the needle close to where the nerve is being pinched or irritated. We’ll then inject a small amount of steroid there, hoping that it’ll remove the inflammation and alleviate their symptoms.
The majority of our patients find improvement in their symptoms after this injection, which is great because it’s very minimally invasive.
Ultimately, though, it’s dictated by a patient’s pathology.
This means that if a patient comes in with a newer injury, they’re often more likely to be able to treat it quickly and never have to see us again, compared to somebody with a long history of back pain who might have a more challenging time in getting lasting pain relief.
How Can You Tell if You Have Sciatica?
Historically, pain that radiates down the leg past at least two joints is usually nerve-related. If they have accompanying symptoms, numbness or paresthesias (a tingling feeling on your skin), that’s probably also nerve-related.
Here’s a nifty little trick to see if you might be suffering from Sciatica or a nerve-related injury (though this isn’t a formal diagnosis). It’s called the positive straight leg raise:
What you’re doing with this bit of physical exam finding is putting tension on the sciatic nerve, which pulls at the root where the irritation is.
Now, this doesn’t give you the exact level or nerve root that’s being irritated. You’ll need more in-depth analysis and an MRI to confirm the inflammation or injury’s actual level.
—
At the end of the day, many sciatica patients have symptoms that resolve on their own. If you think you’re suffering from Sciatica, chronic back pain, or pain coming from your nerves, you can find us here in Texas to help you.