
MILLIONS OF AMERICANS ARE AFFECTED BY SOME FORM OF ARTHRITIS.
Rheumatology Diseases are the most common cause of disability in the United States. Rheumatic disease is not a single disorder, though, as people use the term “rheumatoid arthritis” to refer to all rheumatic ailments.
There are over 200 different diseases under the purview of rheumatology, spanning several types of arthritis and other systemic connective tissue diseases. Other rheumatic diseases are considered autoimmune diseases, meaning that the body’s immune system attacks healthy body tissue by mistake.
When searching for “rheumatology near me” or a “rheumatology doctor in Austin,” trust the specialization of Advanced Pain Care’s dedicated team. We are committed to understanding your unique needs and ensuring you receive the best care for your rheumatologic concerns.
Experience the difference at our center. Book a consultation with us today.
Common Causes of Rheumatic Conditions
Rheumatic conditions are inflammatory with several considered “autoimmune”. While the actual causes of rheumatology diseases are still not clearly understood, some factors can contribute to the early symptoms of certain rheumatic disorders. These include:
- Pre-existing Medical Conditions
- Metabolic Conditions
- Wear and Tear
- Age
- Infections
- Trauma
- Gender
- Environmental Factors
- Genetic Factors
- Lifestyle Choices
- Pre-existing Medical Conditions
- Metabolic Conditions
- Age
- Wear and Tear
- Trauma
- Infections
- Gender
- Environmental Factors
- Genetic Factors
- Lifestyle Choices
Research also suggests that certain ethnic backgrounds are more disposed to developing certain rheumatic conditions. It is important to note that while rheumatologists treat osteoarthritis, it is not classified as a rheumatic disease. This is primarily because osteoarthritis is not caused by inflammation or autoimmune conditions but caused by natural wear and tear on the body.
Our rheumatology specialists consider this nuanced aspect, ensuring a personalized approach that recognizes individual factors influencing the course of treatment.
Signs and Symptoms of Rheumatic Disorders
The rheumatic conditions affecting the human body, and the signs and symptoms potentially indicating these rheumatic conditions are also extremely varied. Some specific rheumatoid symptoms, though, have very clear markers of a rheumatic condition(s).
Several of these characteristic symptoms are:
- Skin rash (in specific conditions such as lupus)
- Stiffness in the joints, especially in the mornings
- Inflammation of the joints
- Pain in the joints
- Low-grade fever
- Anemia
- Reduced movement in the affected regions
- Redness or sensations of warmth
- Tenderness in the affected areas
- Unexplained fatigue
- Weight loss
Not sure if your symptoms indicate the development of a rheumatic disorder? Our rheumatology consultants can help you.
Different Types of Rheumatology Diseases
Rheumatology doctors categorize rheumatologic diseases and disorders under the medical subspecialty of “rheumatology.” The most common condition is rheumatoid arthritis, although several other rheumatic conditions need to be treated specifically by a rheumatologist.
The common rheumatic conditions include:
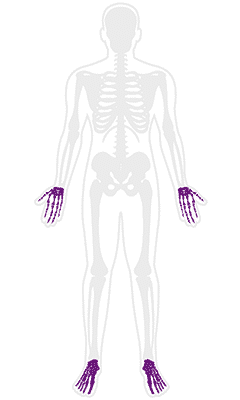
Rheumatoid Arthritis
It is one of the most prevalent health conditions in the United States, affecting over 1.3 million Americans every year. This is why rheumatoid arthritis treatment is a commonly facilitated care in the country.
Primarily characterized by severe inflammation of the joints of the hands and feet, this condition has a long-term prognosis and can lead to chronic pain and disability. Unlike osteoarthritis, rheumatoid arthritis does not occur naturally in the body due to natural wear and tear but instead results from the immune system attacking the body.
Some of the characteristic symptoms of rheumatoid arthritis (RA) include the following:
- Conditions affecting other organs (such as the lungs)
- Pain and inflammation in several joints
- Lumps called rheumatoid nodules
- Joint stiffness
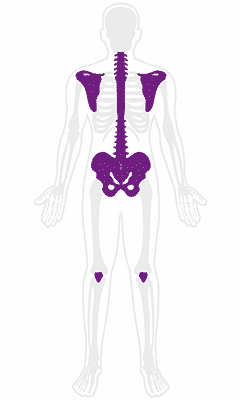
Spondyloarthropathies
A group of diseases that affects the spine, shoulders, knees, and hips, causing inflammation in the ligaments and tendons. People across age groups can experience varied forms of this disease, with symptoms including rashes, mouth sores, and eye issues. One such condition is ankylosing spondylitis.
Ankylosing Spondylitis
A chronic disease that affects the spine and leads to severe pain, inflammation, and stiffness in the lower back. With this condition, the chances of the bones and joints fusing together are high. The joints that are most affected by this condition are the sacroiliac joints.
Some of the characteristic symptoms of ankylosing spondylitis include:
- Severe pain and stiffness in the lower back and buttocks that often improves with activity
- Gradually increasing pain in the middle and upper back regions
- Stiffness in the spine
Psoriatic Arthritis
Another common autoimmune condition that manifests in five variants:
- Arthritis mutilans
- Asymmetric
- Symmetric
- Spondylitis
- Distal
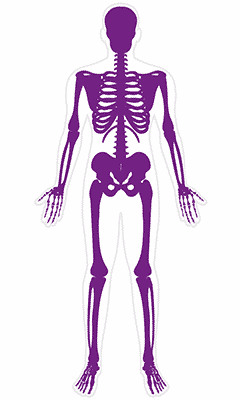
Lupus
Lupus (or systemic lupus erythematosus) is a chronic autoimmune condition that affects joints, muscles, bones, organs, and other parts of the body resulting in severe inflammation of the affected areas.
Common symptoms of lupus also include:
- Blue/white toes and fingers
- Seizures or strokes
- Blood disorders
- Rashes
- Hair loss
Sjogren’s Syndrome
An autoimmune disease with primary symptoms being dryness in the mouth and eyes. This condition is thought to be more common in women.
Primary symptoms of Sjogren’s syndrome include:
- Irritation and burning in the eyes
- Swelling of facial glands
- Decay of the teeth
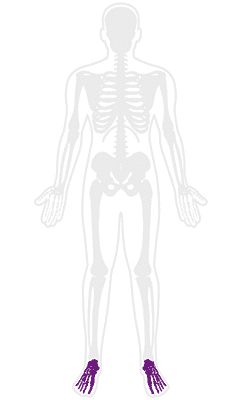
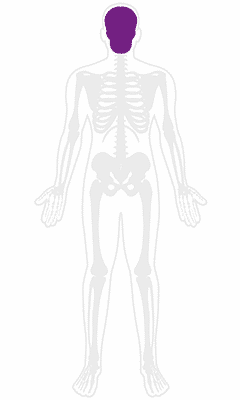
Gout
This condition predominantly occurs in the big toe (or other parts of the feet) and is the result of a build-up of uric acid in the joints. The main symptoms of gout include pain, stiffness, and inflammation in the affected area(s).
Scleroderma
This condition is divided into “localized” scleroderma and “systemic sclerosis. Localized scleroderma hardens the skin (and the structures beneath it) and predominantly affects children. Systemic sclerosis affects organs and blood vessels causing them to harden.
Primary symptoms of scleroderma also include:
- Calcium deposits under the skin
- Raynaud’s phenomenon
- Trouble in digestion
- Thickened skin
- Weak muscles
If you experience any of them, it’s time to make an appointment with an Advanced Pain Care center near you.
Common Forms Of Rheumatic Conditions Also Include.
- Juvenile idiopathic arthritis
- Systemic vasculitis
- Marfan syndrome
- Crohn’s disease
- Tendonitis
- Bursitis
- Polymyalgia rheumatica
- Infectious arthritis
- Reactive arthritis
- Fibromyalgia
- Polymyositis
Patient Testimonial
“I have seen Dr. Pegram for some years now. He is such a caring doctor, and he is extremely knowledgeable. He really listens to me and is very thorough in his examinations while asking me questions. Dr.Pegram orders blood tests and the imaging necessary to address my health problems and to ensure that he makes the right diagnosis. I feel confident and cared for every time I see him. He also NEVER has a foot out the door like other physicians, he takes the time needed to listen to me.
In addition to that, when I mention to another physician that he is my doctor, the doctors volunteer their admiration for him. One doctor even said, “Dr. Pegram is a genius!” In my experience when doctors express their admiration for another doctor, it’s because that doctor is top of the line.
My life fortunately, and unfortunately has given me the opportunity to get to know so many physicians. Dr. Pegram is one of the doctors at the very top of my very long list.
Thank you, Dr.Pegram!“
— Lorena De La Cruz-Blackard
How Can You Find The Right Diagnosis for Rheumatoid Arthritis?
The board-certified physicians and rheumatology specialists at Advanced Pain Care use cutting-edge technology and the latest diagnostic and therapeutic procedures to identify and treat a wide range of rheumatic diseases in a multi-specialty setting.
There is no single test to determine if you have a rheumatic condition so symptoms play a vital role in the rheumatologist’s evaluation to help isolate specific and possible conditions.
DIAGNOSTIC EVALUATION BY ADVANCED PAIN CARE RHEUMATOLOGISTS:
In order to arrive at a detailed understanding of your condition, rheumatologists will evaluate the following parameters:
- Genetic markers for predispositions
- Past medical history
- Exposure to infections
- Lifestyle conditions
- Genetic markers for predispositions
- Past medical history
- Exposure to infections
- Lifestyle conditions
With symptoms playing a major role in identifying your condition, your rheumatologist at Advanced Pain Care will also check for signs of swelling, stiffness, and redness while examining pain indicators. A physical exam will also be done to check for eye problems, range of motion and reflexes, skin rashes, and swollen glands.
ADDITIONAL DIAGNOSIS FOR RHEUMATIC CONDITIONS:
To further hone the diagnostic process, common tests rheumatologists prescribe are:
- Blood Tests — to detect markers of inflammation and antibodies associated with specific conditions – antinuclear antibody (ANA), c-reactive protein (CRP), etc
- Imaging Tests — X-rays, CT scans, MRIs, and ultrasounds are all available to detect fluid build-up, cartilage loss, erosion and tears of structures, and any changes in bone structure(s).
- Blood tests to detect abnormalities in organ functions
- Blood tests to detect the presence of specific proteins and uric acid
Depending on the results of a given test, our rheumatoid specialists may ask for additional tests to isolate a specific condition. Some of the tests might include:
- Anti-cyclic citrullinated peptides (anti-CCP)
- Anti-double-stranded DNA antibody
- Synovial fluid analysis
- Rheumatoid factor
- Biopsy
- Erythrocyte sedimentation rate (ESR)
- Anti-Smith antibody test
- Basic metabolic panel
- HLA-B27
Conditions such as gout, lupus, and Lyme’s disease, are difficult to diagnose as they have several overlapping symptoms. In these cases, rheumatologists will often rely on a thorough evaluation of the symptoms along with the results of any specific tests administered.
Different Types of Treatments Available at Advanced Pain Care, Austin
Treatment for rheumatic conditions primarily involves medications. Some medication is used to reduce pain and inflammation while some work to resolve the condition completely.
Specific conditions are also treated with specific medicines. For example, gout is treated using uric acid-depleting medication and corticosteroids. Lyme disease is treated with antibiotics, and lupus (a chronic condition) is treated with anti-malarial drugs. While most forms of arthritis are chronic, infectious arthritis can be cured with the right medication. More complex conditions, like fibromyalgia, cannot be completely healed and often need a multimodal treatment approach to manage the symptoms.
Our specialists understand the complexities of rheumatology diseases and are committed to guiding you through advanced rheumatology treatments.
The most common medications prescribed for rheumatic conditions include:
- Corticosteroids
- Oral analgesics
- Topical analgesics
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Disease-modifying anti-rheumatic drugs (DMARDs)
- Biologics
- Janus Kinase inhibitors
Additional treatment options for rheumatic conditions include:
- Physical therapy
- Occupational therapy
- Hot and cold therapy
- Exercise
- Use of assistive devices
- Alternative and complementary therapies
- Cognitive behavior therapy
- Surgery
Rheumatologists do not usually perform surgeries; that comes under the purview of Orthopedists. Rheumasurgery or rheumatoid surgery is considered a subfield of orthopedics involving a patient who requires surgical treatment to address their condition(s).
A rheumatologist and an orthopedist are both trained to treat conditions relating to the patient’s joints, muscles, and bones. While a rheumatologist evaluates, diagnoses, and medicinally treats these conditions, an orthopedist specializes in surgical treatments.
Rheumatology
The Rheumatology Specialists At Advanced Pain Care Are Highly Trained to Treat a Variety of Rheumatic Diseases With An Array of Treatment Options.
The type of treatment you receive at our Center for Rheumatology will depend on the severity and extent of your condition and might include medication, joint injections, aspirations, or infusions.
Don’t let rheumatic conditions limit your life—schedule your appointment now and embark on a path to improved health! Discover personalized care and management at Advanced Pain Care. Visit a location near you for more information or call 512-244-4272 to book a same or next-day appointment with one of our rheumatology doctors.
FAQS
Q: What does a rheumatology doctor treat?
A: Rheumatologists, skilled in internal medicine and pediatrics, specialize in treating conditions affecting soft tissues, joints, autoimmune diseases, vasculitis, and genetic connective tissue disorders. Our expert team at Advanced Pain Care in Austin is trained to evaluate and provide treatment plans for autoimmune, inflammatory, and musculoskeletal conditions like rheumatoid arthritis, lupus, ankylosing spondylitis, scleroderma, tendinitis, and sarcoidosis.
Q: What is rheumatology disease?
A: Rheumatic disease refers to several medically diagnosed diseases and disorders that affect the joints, bones, tendons, ligaments, cartilage, and muscles in the human body. Some diseases also affect healthy tissue. They are also referred to as autoimmune diseases, and a rheumatologist is a specialist who diagnoses and treats these specific conditions. Other rheumatic diseases are also considered “autoimmune diseases”, which means the body’s immune system attacks healthy body tissue by mistake.
With over 200 different diseases falling under rheumatology’s purview, our specialists at Advanced Pain Care in Austin address various types of arthritis, osteoporosis, and systemic connective tissue diseases.
Q: What diseases do rheumatologists diagnose?
A: Some of the common rheumatic diseases and disorders diagnosed by rheumatologists are:
- Rheumatoid arthritis
- Ankylosing spondylitis
- Bursitis
- Sarcoidosis
- Tendinitis
- Gout
- Juvenile Idiopathic arthritis
- Septic arthritis
- Crohn’s disease
- Osteoporosis
Our specialists at Advanced Pain Care, Austin, ensure personalized and thorough care planned to meet the needs of your unique condition.
Q: What does rheumatism pain feel like?
A:Rheumatologists, skilled in internal medicine and pediatrics, specialize in treating conditions affecting soft tissues, joints, autoimmune diseases, vasculitis, and genetic connective tissue disorders. Our expert team at Advanced Pain Care in Austin is trained to evaluate and provide treatment plans for autoimmune, inflammatory, and musculoskeletal conditions like rheumatoid arthritis, lupus, ankylosing spondylitis, scleroderma, tendinitis, and sarcoidosis.
Q: What does rheumatism pain feel like?
A: Rheumatic pain is a localized pain experienced in the affected joints, tissues, muscles, tendons, and bones. The pain is usually experienced as a deep and aching sensation or as a soreness. While the severity of the pain differs among people, “arthritic pain” is not considered to be as severe as “neuropathic pain”, “visceral pain”, or “ischemic pain”. As these symptoms are accompanied by stiffness, soreness, redness, and reduced motion, our team at Advanced Pain Care provides solutions for managing and alleviating rheumatism pain.
Q: What is the difference between a rheumatologist and an orthopedist?
A: A rheumatologist and an orthopedist are both trained to treat conditions relating to the patient’s joints, muscles, and bones. A rheumatologist evaluates, diagnoses, and medically treats rheumatic diseases and conditions, and orthopedists specialize in surgical treatments for the treatment of these conditions. At our multispecialty pain care center, we ensure you receive the appropriate care to live the life you desire.
Q: Can children develop rheumatic diseases?
A: Yes, children can develop rheumatic diseases. Juvenile idiopathic arthritis (JIA) is one of the most common rheumatic diseases in children. Other rheumatic conditions affecting children include juvenile lupus, juvenile dermatomyositis, and juvenile scleroderma.


